
A Tragic Spring Farm Fire and the Imperative for Stronger Safety Frameworks in Disability Housing
Sadly, as I predicted in my Blog Post on October
In late August 2011, a magnitude 5.8 earthquake – the strongest east of the Mississippi since 1944 – shook Washington, D.C., with such force that it cracked the Washington Monument and damaged the National Cathedral.
 On the sixth floor of the neonatal intensive care unit (NICU) at Children’s National in Washington, D.C., staff felt the hospital swaying from side to side.
On the sixth floor of the neonatal intensive care unit (NICU) at Children’s National in Washington, D.C., staff felt the hospital swaying from side to side.
After the shaking stopped, they found the natural disaster exposed another fault: The unit’s 200-plus staff members were not all equally knowledgeable or confident regarding the unit’s plan for evacuating its 66 newborns or their own specific role during an emergency evacuation.
More than 900 very sick children are transferred to Children’s National NICU from across the region each year, and a high percentage rely on machines to do the work that their tiny lungs and hearts are not yet strong enough to do on their own.
Transporting fragile babies down six flights of stairs along with vital equipment that keeps them alive requires planning, teamwork and training.
“Fires, tornadoes and other natural disasters are outside of our team’s control. But it is within our team’s control to train NICU staff to master this necessary skill,” says Lisa Zell, BSN, a clinical educator. Zell is also lead author of a Children’s National article featured on the cover of the July/September 2019 edition of The Journal of Perinatal & Neonatal Nursing. “Emergency evacuations trigger safety concerns for patients as well as our own staff. A robust preparedness plan that is continually improved can alleviate such fears,” Zell adds.
Children’s National is the nation’s No. 1 NICU, and its educators worked with a diverse group within Children’s National to design and implement periodic evacuation simulations. From June 2015 to August 2017, 213 members of NICU staff took part in simulated drills, honing their skills by practising with mannequins with varying levels of acuity.

The two-hour evacuation simulation training at Children’s National begins with a group prebriefed. During this meeting, NICU educators discuss the overarching evacuation plan, outline individual roles and give a hands-on demonstration of all of the evacuation equipment.
This equipment includes emergency backpacks, a drip calculation sheet and an emergency phrase card. Emergency supply backpacks are filled with everything that each patient needs post evacuation, from suction catheters, butterfly needles and suture removal kits to flashlights with batteries.
Each room is equipped with that emergency backpack which is secured in a locked cabinet. Every nurse has a key to access the cabinet at any time.
Vertical evacuation scenarios are designed to give trainees a real-world experience. Mannequins that are intubated are evacuated by tray, allowing the nurse to provide continuous oxygen with the use of a resuscitation bag during the evacuation. Evacuation by sled allows three patients to be transported simultaneously. Patients with uncomplicated conditions can be lifted out of their cribs and swiftly carried to safety.
Teams also learn how to calm the nerves of frazzled parents and enlist their help. “Whatever we need to do, we will to get these babies out alive,” Joan Paribello, a clinical educator, tells 15 staff assembled for a recent pre-briefing session.

The simulated training ends with a debrief session during which issues that arose during the evacuation are identified and corrected prior to subsequent simulated trainings, improving the safety and expediency of the exercise.
Indeed, as Children’s National NICU staff mastered these evacuation simulations, evacuation times dropped from 21 minutes to as little as 16 minutes. Equally important, post evacuation surveys indicate:
“One of the most surprising revelations regarded one of the most basic functions in any NICU,” Dr. Soghier adds. “Once intravenous tubing is removed from its pump, the rate at which infusions drip needs to be calculated manually. We created laminated cards with pre-calculated drip rates to enable life-saving fluid delivery to continue without interruption.”

Sadly, as I predicted in my Blog Post on October
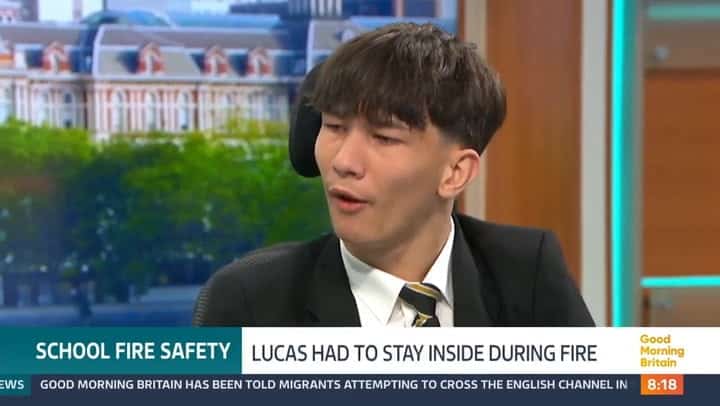
The fire alarm in his UK school starts blaring while smoke rises

Challenging the Status Quo: Building Classifications and Fire Safety in